Interventional Pulmonology
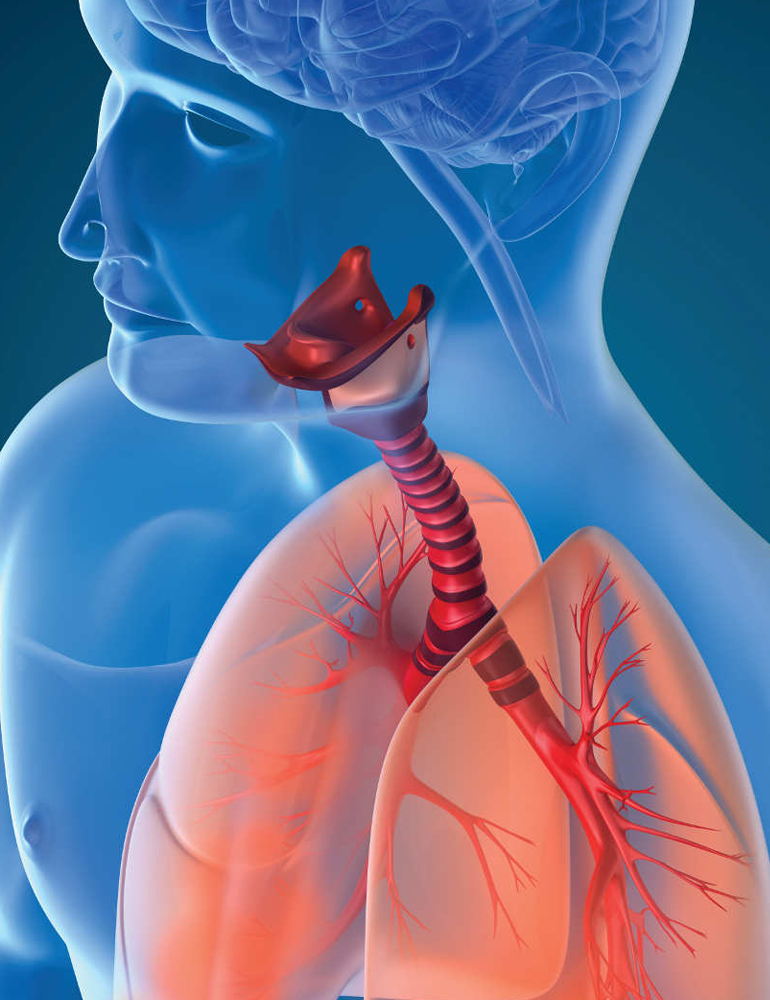
Interventional pulmonology is a subspecialty of pulmonary medicine that focuses on the diagnosis and treatment of diseases of the lungs and airways using minimally invasive techniques. It combines the principles of pulmonology (respiratory medicine) and interventional radiology to provide advanced diagnostic and therapeutic procedures for various lung conditions.
Interventional pulmonologists are highly trained physicians who have expertise in bronchoscopy and other minimally invasive procedures to diagnose and treat a wide range of lung disorders. They use specialized instruments and imaging techniques to access and treat abnormalities within the respiratory system.
Here are some common procedures performed by interventional pulmonologists:
- Bronchoscopy: This is a procedure in which a thin, flexible tube called a bronchoscope is inserted through the mouth or nose and into the airways. It allows the physician to visualize the inside of the airways, take tissue samples (biopsies), remove foreign objects, and treat various conditions such as tumors, infections, and blockages.
- Transbronchial Needle Aspiration (TBNA): TBNA is a technique used to obtain tissue or fluid samples from lymph nodes or masses located near the airways. A needle is passed through the bronchoscope to collect samples for further analysis.
- Endobronchial Ultrasound (EBUS): EBUS combines bronchoscopy with ultrasound imaging to visualize the structures around the airways, such as lymph nodes or tumors. It helps in obtaining tissue samples for diagnosing lung cancer and staging the disease.
- Pleuroscopy and Thoracoscopy: These procedures involve inserting a thin tube with a camera (thoracoscope) into the chest cavity through small incisions. They allow the visualization and evaluation of the pleura (lining of the lungs) and pleural space. These techniques are used in the diagnosis and treatment of conditions such as pleural effusions (accumulation of fluid), pleural tumors, and pneumothorax (collapsed lung).
- Airway Stenting: Stents are used to open narrowed or blocked airways caused by tumors, strictures, or other conditions. They are placed during bronchoscopy to maintain airway patency and improve breathing.
Immunology
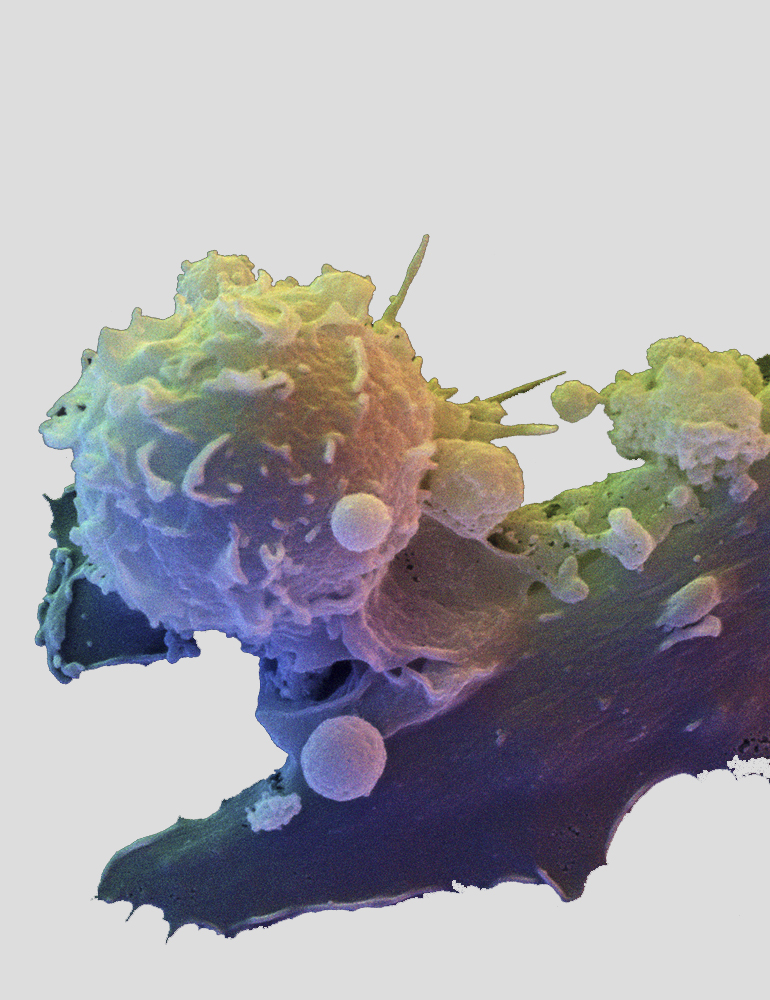
Immunology is the branch of biomedical science that deals with the study of the immune system, which is the complex network of cells, tissues, and molecules that work together to defend the body against harmful pathogens, such as bacteria, viruses, parasites, and fungi. It also plays a crucial role in recognizing and eliminating abnormal cells, including cancer cells.
The immune system has two main components: the innate immune system and the adaptive immune system. The innate immune system provides immediate, nonspecific defense mechanisms, while the adaptive immune system mounts a specific response tailored to a particular pathogen.
Key concepts and components in immunology include:
- Antigens: Antigens are substances that can elicit an immune response. They are usually proteins or large carbohydrates found on the surface of pathogens or abnormal cells. When the immune system encounters an antigen, it recognizes it as foreign and initiates an immune response.
- Antibodies: Antibodies, also known as immunoglobulins, are specialized proteins produced by certain white blood cells called B cells. Antibodies recognize and bind to specific antigens, marking them for destruction by other components of the immune system.
- Lymphocytes: Lymphocytes are a type of white blood cell that plays a central role in the immune response. There are two main types of lymphocytes: B cells and T cells. B cells are responsible for producing antibodies, while T cells have various functions, including directly killing infected cells and coordinating immune responses.
- Major Histocompatibility Complex (MHC): MHC molecules are proteins found on the surface of most cells in the body. They play a crucial role in presenting antigens to T cells, allowing the immune system to distinguish between self and non-self cells.
- Cytokines: Cytokines are small signaling molecules secreted by various cells of the immune system. They regulate immune responses by facilitating communication between immune cells and promoting inflammation, cell growth, and differentiation.
- Immunological Memory: One of the key features of the adaptive immune system is its ability to develop immunological memory. After an initial exposure to a specific pathogen, the immune system "remembers" the pathogen, enabling a faster and more robust response upon subsequent encounters. This is the basis for vaccination, which harnesses the immune system's memory to provide protection against future infections.
Immunology encompasses a wide range of research areas and applications, including the study of immune-related disorders (such as autoimmune diseases, allergies, and immunodeficiencies), vaccine development, transplantation immunology, cancer immunotherapy, and the role of the immune system in infectious diseases. Understanding immunology is crucial for developing effective treatments, therapies, and preventive strategies to combat diseases and promote human health.
Pleural Disease
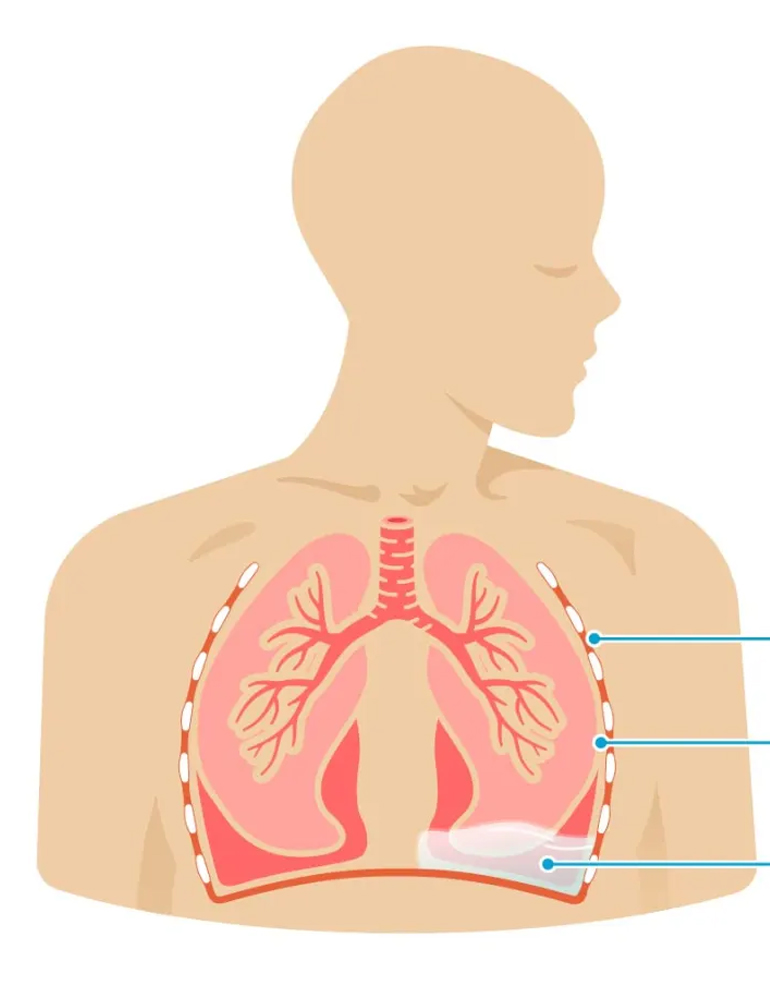
Pleural disease refers to conditions that affect the pleura, which is the thin membrane that lines the surface of the lungs and the inside of the chest cavity. The pleura consists of two layers: the visceral pleura, which covers the lungs, and the parietal pleura, which lines the chest wall.
There are several types of pleural diseases, including:
- Pleural Effusion: Pleural effusion is the accumulation of excess fluid in the pleural space, the space between the two layers of the pleura. It can be caused by various factors, including infections, heart failure, malignancies (such as lung cancer), liver disease, kidney disease, and inflammation. Symptoms may include chest pain, shortness of breath, coughing, and reduced lung function. Treatment involves addressing the underlying cause and may include draining the fluid with a needle or tube (thoracentesis) or using medications to prevent further fluid accumulation.
- Pneumothorax: Pneumothorax occurs when air accumulates in the pleural space, causing the lung to collapse partially or completely. It can result from lung diseases (such as emphysema), trauma to the chest, certain medical procedures, or occur spontaneously without an obvious cause. Symptoms include sudden chest pain, shortness of breath, and rapid breathing. Treatment options depend on the severity of the pneumothorax and may include observation, aspiration of air with a needle, or insertion of a chest tube to remove the air and allow the lung to re-expand.
- Pleurisy: Pleurisy, also known as pleuritis, is inflammation of the pleura. It is often caused by viral or bacterial infections, such as pneumonia or tuberculosis, but can also result from autoimmune disorders (e.g., rheumatoid arthritis, lupus), pulmonary embolism, or certain medications. Pleurisy is characterized by sharp chest pain that worsens with breathing or coughing. Treatment focuses on addressing the underlying cause and managing symptoms with pain medications and anti-inflammatory drugs.
- Pleural Thickening: Pleural thickening refers to the abnormal thickening and scarring of the pleural membranes. It can be a consequence of long-standing inflammation, asbestos exposure (asbestosis), previous infections, or other lung diseases. Pleural thickening can restrict lung expansion and lead to breathing difficulties. Treatment depends on the severity and underlying cause but may involve managing symptoms and addressing the underlying condition if possible.
- Pleural Tumors: Tumors can develop within the pleura, either originating from the pleura itself (primary pleural tumors) or spreading from other organs (metastatic tumors). Malignant pleural mesothelioma, often associated with asbestos exposure, is an example of a primary pleural tumor. Treatment options include surgery, radiation therapy, chemotherapy, and targeted therapies, depending on the type and stage of the tumor.
The diagnosis of pleural diseases often involves a combination of medical history evaluation, physical examination, imaging tests (such as chest X-rays or CT scans), and analysis of pleural fluid samples. Treatment approaches vary depending on the specific condition and its underlying cause but may involve medications, minimally invasive procedures, or surgery.

Critical Care
Critical care, also known as intensive care, refers to specialized medical care provided to individuals who are critically ill, injured, or in a life-threatening condition. It involves close monitoring, advanced life support interventions, and comprehensive management of organ system failure to stabilize and improve the patient's condition.
Critical care units, commonly referred to as intensive care units (ICUs), are equipped with specialized medical equipment and staffed by a multidisciplinary team of healthcare professionals with expertise in critical care medicine. This team typically includes intensivists (doctors specialized in critical care), nurses, respiratory therapists, pharmacists, nutritionists, and other healthcare professionals.
Here are some key aspects of critical care:
- Patient Monitoring: Critical care patients require continuous monitoring of vital signs, such as heart rate, blood pressure, oxygen saturation, and respiratory rate. Advanced monitoring techniques, including invasive monitoring such as arterial catheters, central venous catheters, and pulmonary artery catheters, may be used to assess the patient's hemodynamic status and organ function.
- Life Support: Critical care often involves the use of life-sustaining interventions and technologies to support vital functions. These may include mechanical ventilation to assist with breathing, hemodynamic support with medications and intravenous fluids, renal replacement therapy (dialysis) for kidney failure, and other techniques to support failing organ systems.
- Multisystem Organ Support: Critical care addresses the needs of patients with multiple organ dysfunction or failure. It focuses on maintaining or restoring organ function through appropriate interventions and therapies. This may involve optimizing cardiovascular function, managing fluid balance, ensuring adequate oxygenation, and providing nutritional support.
- Infection Control: Infections are a common concern in the critical care setting. Strict infection control measures, including hand hygiene, sterile techniques, and appropriate use of antibiotics, are implemented to prevent and manage infections. Additionally, isolation precautions may be necessary to prevent the spread of infectious diseases.
- Team-Based Approach: Critical care involves a multidisciplinary team approach, with healthcare professionals from various specialties working together to provide comprehensive care. The team collaborates to make complex decisions, manage treatment plans, and ensure optimal patient outcomes.
Common conditions that may require critical care include severe respiratory distress or failure, sepsis or severe infections, major trauma, cardiac emergencies, neurological emergencies, and postoperative care for high-risk surgeries.
Critical care aims to stabilize and improve the patient's condition while addressing the underlying causes of the critical illness. Once the patient's condition stabilizes, they may be transferred to a lower acuity care unit or step-down unit for continued monitoring and recovery.

Allergy Asthma
Allergy asthma, also known as allergic asthma, is a type of asthma that is triggered by exposure to specific allergens. Asthma is a chronic respiratory condition characterized by inflammation and narrowing of the airways, resulting in symptoms such as wheezing, coughing, shortness of breath, and chest tightness. Allergic asthma is one of the most common forms of asthma, and it is closely linked to allergic reactions.
Here are some key points about allergy asthma:
- Allergens: Allergens are substances that can trigger an allergic response in susceptible individuals. Common allergens associated with allergy asthma include pollen from trees, grasses, and weeds, dust mites, pet dander, mold spores, and certain food allergens. When a person with allergic asthma is exposed to these allergens, their immune system overreacts, leading to inflammation and constriction of the airways.
- Immune Response: In allergic asthma, the immune system's response to allergens involves the production of an antibody called immunoglobulin E (IgE). IgE binds to the allergens, triggering the release of inflammatory chemicals, such as histamine, in the airways. This causes swelling, mucus production, and constriction of the bronchial tubes, leading to asthma symptoms.
- Symptoms: Allergic asthma symptoms are similar to those of other types of asthma and may include wheezing (a whistling sound during breathing), coughing (especially at night or early morning), shortness of breath, chest tightness, and difficulty in performing physical activities. These symptoms can vary in severity and frequency.
- Diagnosis: The diagnosis of allergic asthma typically involves a thorough medical history, physical examination, and lung function tests, such as spirometry, to assess the airflow obstruction. Allergy testing may also be conducted to identify specific allergens that trigger the symptoms.
- Treatment: The management of allergic asthma aims to control symptoms, prevent asthma attacks, and improve lung function.

Tuberculosis
Tuberculosis (TB) is a contagious infectious disease caused by the bacterium Mycobacterium tuberculosis. It primarily affects the lungs but can also involve other parts of the body, such as the kidneys, spine, and brain. TB is a major global health concern, with millions of new cases reported each year.
Here are some key points about tuberculosis:
- Transmission: TB is spread through the air when an infected individual coughs, sneezes, or speaks, releasing tiny droplets containing the bacteria. People nearby can inhale these droplets and become infected. However, not everyone infected with TB bacteria becomes sick. There are two forms of TB infection: latent TB infection (LTBI) and active TB disease.
- Symptoms: Active TB disease can present with various symptoms, which primarily affect the respiratory system. Common symptoms include a persistent cough lasting more than two weeks, coughing up blood, chest pain, fatigue, weight loss, fever, night sweats, and loss of appetite. However, TB can also affect other organs, leading to symptoms specific to those areas.
- Treatment: TB is treatable with appropriate medications. The standard treatment for active TB disease involves a combination of antibiotics taken for a prolonged period (usually six to nine months or more) to ensure complete eradication of the bacteria. It is essential to complete the full course of treatment to prevent the development of drug-resistant strains and potential relapse. Latent TB infection can be treated with a shorter course of medications to prevent the development of active TB disease.
- Prevention: TB prevention strategies focus on identifying and treating individuals with active TB disease promptly, as well as screening and treating those with latent TB infection who are at higher risk of progression to active disease. Other preventive measures include improving living conditions, implementing infection control measures in healthcare settings, promoting awareness and education about TB, and ensuring access to quality healthcare services.

Sleep Medicine
Sleep medicine is a medical specialty that focuses on the diagnosis, treatment, and management of sleep disorders. Sleep disorders are conditions that affect a person's ability to have quality, restful sleep, leading to daytime fatigue, impaired functioning, and other health issues.
Here are some key aspects of sleep medicine:
- Sleep Disorders: Sleep medicine addresses various sleep disorders, including:
- Insomnia: Difficulty falling asleep, staying asleep, or experiencing non-restorative sleep.
- Sleep Apnea: Interruptions in breathing during sleep due to partial or complete obstruction of the airway.
- Narcolepsy: A neurological disorder characterized by excessive daytime sleepiness and sudden, uncontrollable episodes of sleep.
- Restless Legs Syndrome (RLS): An uncomfortable sensation in the legs accompanied by an urge to move, often disrupting sleep.
- Circadian Rhythm Disorders: Conditions that disrupt the normal sleep-wake cycle, such as shift work sleep disorder or jet lag.
- Parasomnias: Abnormal behaviors or experiences during sleep, including sleepwalking, night terrors, and sleep-related eating disorder.
- REM Sleep Behavior Disorder (RBD): Acting out dreams during REM sleep, which is typically associated with muscle paralysis.
- Sleep-related movement disorders: Conditions characterized by abnormal movements during sleep, such as periodic limb movement disorder (PLMD) or restless legs syndrome (RLS).
- Diagnosis: Sleep disorders are diagnosed through a combination of medical history evaluation, sleep assessments, and diagnostic tests. These may include:
- Polysomnography (PSG): A comprehensive sleep study that involves monitoring brain activity, eye movements, muscle activity, heart rhythm, and respiratory function during sleep. PSG is often conducted in a sleep laboratory or specialized sleep center.
- Home Sleep Testing (HST): Portable devices that measure specific sleep parameters (e.g., breathing, oxygen levels) in the comfort of the patient's home. HST is typically used for diagnosing sleep apnea.
- Multiple Sleep Latency Test (MSLT): A daytime test that measures how quickly a person falls asleep in a quiet environment, assessing excessive daytime sleepiness and diagnosing disorders like narcolepsy.
- Treatment: Sleep medicine employs various treatment approaches based on the specific sleep disorder and individual needs. Treatment options may include:
- Lifestyle Modifications: Implementing healthy sleep habits, such as maintaining a consistent sleep schedule, creating a conducive sleep environment, and practicing relaxation techniques.
- Continuous Positive Airway Pressure (CPAP): A common treatment for sleep apnea, involving the use of a machine that delivers a continuous flow of air through a mask, helping to keep the airway open during sleep.
- Oral Appliances: Custom-fitted devices worn in the mouth to reposition the jaw and tongue, helping to keep the airway open for individuals with sleep apnea.
- Medications: Certain medications may be prescribed to address specific sleep disorders, such as insomnia, restless legs syndrome, or narcolepsy. However, medication use is typically complemented with other treatment strategies.
- Cognitive Behavioral Therapy for Insomnia (CBT-I): A structured therapy that addresses the psychological and behavioral factors contributing to insomnia and promotes healthy sleep patterns.
- Light Therapy: Used to regulate the sleep-wake cycle in circadian rhythm disorders by exposing individuals to specific wavelengths of light at certain times of the day.
- Surgery: In some cases of sleep apnea, surgical interventions may be considered to remove obstructions or correct anatomical abnormalities in the upper airway.
- Sleep Hygiene Education: Sleep medicine practitioners also focus on educating patients about sleep hygiene, which refers to adopting behaviors and practices that promote good sleep quality.

Respiratory Disease
Respiratory diseases are conditions that affect the respiratory system, which includes the organs involved in breathing. These diseases can impact the lungs, airways, and other components of the respiratory system, leading to a range of symptoms and health complications. Here are some common respiratory diseases:
- Asthma: A chronic condition characterized by inflammation and narrowing of the airways, causing recurring episodes of wheezing, coughing, shortness of breath, and chest tightness. Asthma can be triggered by allergens, irritants, exercise, or respiratory infections.
- Chronic Obstructive Pulmonary Disease (COPD): A progressive lung disease that includes chronic bronchitis and emphysema. COPD causes airflow limitation, leading to symptoms such as chronic cough, sputum production, shortness of breath, and reduced exercise tolerance. Smoking is the primary cause of COPD, but long-term exposure to air pollutants can also contribute.
- Pneumonia: An infection of the lungs typically caused by bacteria, viruses, or fungi. Pneumonia leads to inflammation in the air sacs, causing symptoms such as cough, fever, chest pain, and difficulty breathing. The severity of pneumonia can range from mild to life-threatening, particularly in vulnerable populations.
- Tuberculosis (TB): An infectious disease caused by Mycobacterium tuberculosis. TB primarily affects the lungs but can also impact other organs. Symptoms include persistent cough, coughing up blood, weight loss, fatigue, fever, and night sweats. TB is a global health concern, and proper diagnosis and treatment are essential to prevent its spread.
- Respiratory Allergies: Conditions such as allergic rhinitis (hay fever) and allergic conjunctivitis involve an allergic reaction to airborne allergens like pollen, dust mites, pet dander, or mold spores. Symptoms include sneezing, runny or stuffy nose, itchy or watery eyes, and nasal congestion.
- Pulmonary Fibrosis: A group of lung diseases characterized by the progressive scarring and thickening of lung tissues, impairing their ability to function properly. Pulmonary fibrosis leads to symptoms such as shortness of breath, dry cough, fatigue, and chest discomfort.
- Pulmonary Embolism: A condition where a blood clot (usually from the leg) travels to the lungs, obstructing blood flow. Symptoms include sudden-onset shortness of breath, chest pain, cough, and rapid heartbeat. Pulmonary embolism is a medical emergency requiring immediate attention.
- Lung Cancer: The uncontrolled growth of abnormal cells in the lung tissues, leading to the formation of tumors. Lung cancer is often linked to smoking but can also occur in non-smokers. Symptoms include persistent cough, chest pain, weight loss, coughing up blood, and shortness of breath.
- Sleep-Related Breathing Disorders: Conditions like obstructive sleep apnea (OSA) involve repeated partial or complete obstruction of the upper airway during sleep, leading to disrupted sleep and low oxygen levels. Symptoms include loud snoring, excessive daytime sleepiness, morning headaches, and poor concentration.
- Cystic Fibrosis: A genetic disorder that affects multiple organs, including the lungs. It causes the production of thick, sticky mucus that obstructs the airways, leading to recurrent lung infections, cough, shortness of breath, poor growth, and digestive problems.

Chronic Cough
A chronic cough is a cough that lasts eight weeks or longer in adults, or four weeks in children.
A chronic cough is more than just an annoyance. A chronic cough can interrupt your sleep and leave you feeling exhausted. Severe cases of chronic cough can cause vomiting, lightheadedness and even rib fractures.
While it can sometimes be difficult to pinpoint the problem that's triggering a chronic cough, the most common causes are tobacco use, postnasal drip, asthma and acid reflux. Fortunately, chronic cough typically disappears once the underlying problem is treated.
Symptoms
A chronic cough can occur with other signs and symptoms, which may include:
- A runny or stuffy nose
- A feeling of liquid running down the back of your throat (postnasal drip)
- Frequent throat clearing and sore throat
- Hoarseness
- Wheezing and shortness of breath
- Heartburn or a sour taste in your mouth
- In rare cases, coughing up blood